Gene-level Studies
Epidemiological studies and genome-wide association studies (GWAS) of DNA variation with disease have identified numerous genetic risk variants for Alzheimer’s disease. These genetic risk factors provide powerful model systems for unraveling some of the molecular and cellular mechanisms underlying Alzheimer’s disease and for identifying therapeutic strategies tailored to a patient’s genetic makeup. After employing RNA sequencing to reveal cellular programs impacted by the risk factor, my lab uses sophisticated and highly tractable in vitro systems to dissect the underlying mechanisms.
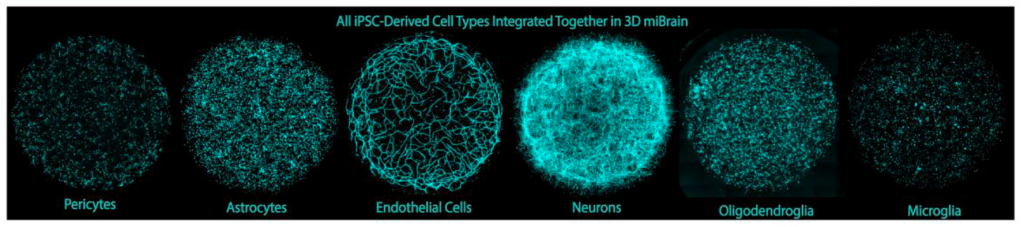
iPSC-derived in vitro systems
Many of our in vitro systems are built from induced pluripotent stem cells (iPSC) derived from patients harboring a specific risk variant. These iPSC can be differentiated into different brain cell types, and isogenic control cells that share the exact genetic background and differ only at the risk position can be generated by precise DNA editing using CRISPR/Cas9 technology. Our in vitro models range from monocultures of individual cell types to complex co-culture systems modeling the brain vasculature [1], myelinated neuronal axons [2], or even a complete vascularized brain tissue [3]. The modular assembly of these co-culture systems allows “mixing and matching” of brain cell types with and without a risk factor, so that the effect of risk variants in a specific cell type can be isolated. In addition, our iPSC-derived in vitro systems enable live imaging using fluorescent biosensors for real-time monitoring of molecular processes or efficient drug screening.
Cell-type specific effects of APOE4
The ε4 allele in the APOE gene is the strongest known genetic risk factor for non-familial Alzheimer’s disease. APOE codes for apolipoprotein E (ApoE), the major protein component of high-density lipoprotein particles in the brain that transport cholesteryl ester and fatty acids between cells. Our transcriptomic studies in postmortem samples from Alzheimer’s patients with and without the APOE4 genotype indicated that presence of APOE4 leads to expression differences for genes associated with lipid metabolism and storage. In follow-up studies using our iPSC-based in vitro systems, we found that presence of the APOE4 allele causes glial accumulation of lipid droplets [2,4,5], small intracellular organelles that store fatty acids in the form of triacylglycerides and cholesteryl ester. Interestingly, this lipid-burdened phenotype in glial cells had been described by Alzheimer himself in his first description of the disease named after him.
Candidate therapeutics for APOE4 effects
Using our iPSC-based in vitro systems, we also identified several different agents that could resolve this APOE4-associated lipid droplet accumulation and related effects in glial cells. In APOE4 astrocytes, supplementation with CDP-choline, a widely available nutritional supplement and the rate limiting intermediate in the synthesis of the membrane lipid phosphatidylcholine, resolved the lipid droplet accumulation [4]. In APOE4 oligodendrocytes, treatment with cyclodextrin abolished both lipid droplet accumulation and myelination defects associated with a redistribution of cholesterol from myelin sheaths around neuronal axons to lipid droplets in the cell bodies [2]. Cyclodextrin, a cyclic polysaccharide that is commonly used as a solubilizer in the food and drug industry, presumably normalizes myelination by APOE4 oligodendrocytes by promoting the redistribution of cholesterol within the cell. Treatment with cyclodextrin also improved learning and executive function in transgenic mice expressing human ApoE with the APOE4 allele, further supporting its therapeutic potential. In APOE4 microglia, lipid droplet accumulation is accompanied by an activated phenotype and a weakened response to neuronal cues mediated by the purinergic P2RY12 receptor [5]. Inhibiting fatty acid synthesis with Triacsin C resolved this lipid droplet accumulation and restored microglial responsiveness to neuronal cues.
Cell-type specific effects of loss-of-function variants in ABCA7
Loss-of-function variants in ABCA7 are also associated with a strong genetic risk for non-familial Alzheimer’s disease. ABCA7 is a membrane protein that effluxes lipids to ApoE in lipoprotein particles and flips phospholipids from the inner to the outer leaflet of the plasma and other membranes. Our transcriptomic studies in postmortem samples from Alzheimer’s patients revealed a metabolic shift away from phosphatidylcholine synthesis towards triacylglyceride accumulation in neurons with ABCA7 loss of function [6]. iPSC-derived neurons with ABCA7 loss of function indeed showed accumulation of lipid droplets and also displayed dysregulation of the mitochondrial membrane potential, indicating a decreased ability to metabolize lipids. Promoting phosphatidylcholine synthesis by supplementation with CDP-choline resolved lipid droplet accumulation and normalized the mitochondrial membrane potential. These findings indicate that lipid dysregulation is not limited to glial cells harboring the APOE4 allele but may play a wider role in Alzheimer’s pathogenesis. In addition, the findings further support the potential of choline supplementation as a therapeutic for Alzheimer’s disease.
References
- Blanchard, Joel W., Michael Bula, Jose Davila-Velderrain, Leyla Anne Akay, Lena Zhu, Alexander Frank, Matheus B. Victor, et al. 2020. “Reconstruction of the human blood–brain barrier in vitro reveals a pathogenic mechanism of APOE4 in pericytes.” Nature Medicine 26 (6): 952–63.
- Blanchard, Joel W., Leyla Anne Akay, Jose Davila-Velderrain, Djuna von Maydell, Hansruedi Mathys, Shawn M. Davidson, Audrey Effenberger, et al. 2022. “APOE4 Impairs Myelination via Cholesterol Dysregulation in Oligodendrocytes.” Nature 611 (7937): 769–79.
- Stanton, Alice E., Adele Bubnys, Emre Agbas, Benjamin James, Dong Shin Park, Alan Jiang, Rebecca L. Pinals, et al. 2024. “Engineered 3D Immuno-Glial-Neurovascular Human miBrain Model.” bioRxiv : The Preprint Server for Biology, June. https://doi-org.ezproxy.canberra.edu.au/10.1101/2023.08.15.553453.
- Sienski, Grzegorz, Priyanka Narayan, Julia Maeve Bonner, Nora Kory, Sebastian Boland, Aleksandra A. Arczewska, William T. Ralvenius, et al. 2021. “APOE4 Disrupts Intracellular Lipid Homeostasis in Human iPSC-Derived Glia.” Science Translational Medicine 13 (583). https://doi-org.ezproxy.canberra.edu.au/10.1126/scitranslmed.aaz4564.
- Victor, Matheus B., Noelle Leary, Xochitl Luna, Hiruy S. Meharena, Aine Ni Scannail, P. Lorenzo Bozzelli, George Samaan, et al. 2022. “Lipid accumulation induced by APOE4 impairs microglial surveillance of neuronal-network activity.” Cell Stem Cell 29 (8): 1197-1212.e8.
- Maydell, Djuna von, Shannon Wright, Julia Maeve Bonner, Colin Staab, Andrea Spitaleri, Liwang Liu, Ping-Chieh Pao, et al. 2024. “Single-Cell Atlas of ABCA7 Loss-of-Function Reveals Impaired Neuronal Respiration via Choline-Dependent Lipid Imbalances.” Org: The Preprint Server for Biology, June. https://doi-org.ezproxy.canberra.edu.au/10.1101/2023.09.05.556135.